//
Evaluation of the Video Ocular Counter-Roll (vOCR) as a New Clinical Test of Otolith Function in Peripheral Vestibulopathy
Search
Try Notion
Evaluation of the Video Ocular Counter-Roll (vOCR) as a New Clinical Test of Otolith Function in Peripheral Vestibulopathy
Authors text
Sadeghpour, Shirin, Fornasari, Francesco, Otero-Millan, Jorge, Carey, John P, Zee, David S, Kheradmand, Amir
Journal/Book
JAMA otolaringology
Year
2021
Abstract
Importance Video-oculography (VOG) goggles have been integrated into the assessment of semicircular canal function in patients with vestibular disorders. However, a similar bedside VOG method for testing otolith function is lacking.
Objective To evaluate the use of VOG-based measurement of ocular counter-roll (vOCR) as a clinical test of otolith function.
Design, Setting, and Participants A case-control study was conducted to compare vOCR measurement among patients at various stages of unilateral loss of vestibular function with healthy controls. The receiver operating characteristic curve method was used to determine the diagnostic accuracy of the vOCR test in detecting loss of otolith function. Participants were recruited at a tertiary center including the Johns Hopkins outpatient clinic and Johns Hopkins Hospital, Baltimore, Maryland. Participants included 56 individuals with acute (≤4 weeks after surgery), subacute (4 weeks-6 months after surgery), and chronic (>6 months after surgery) unilateral vestibular loss as well as healthy controls. A simple bedside maneuver with en bloc, 30° lateral tilt of the head and trunk was used for vOCR measurement. The study was conducted from February 2, 2017, to March 10, 2019.
Intervention In each participant vOCR was measured during static tilts of the head and trunk en bloc.
Main Outcomes and Measures The vOCR measurements and diagnostic accuracy of vOCR in detecting patients with loss of vestibular function from healthy controls.
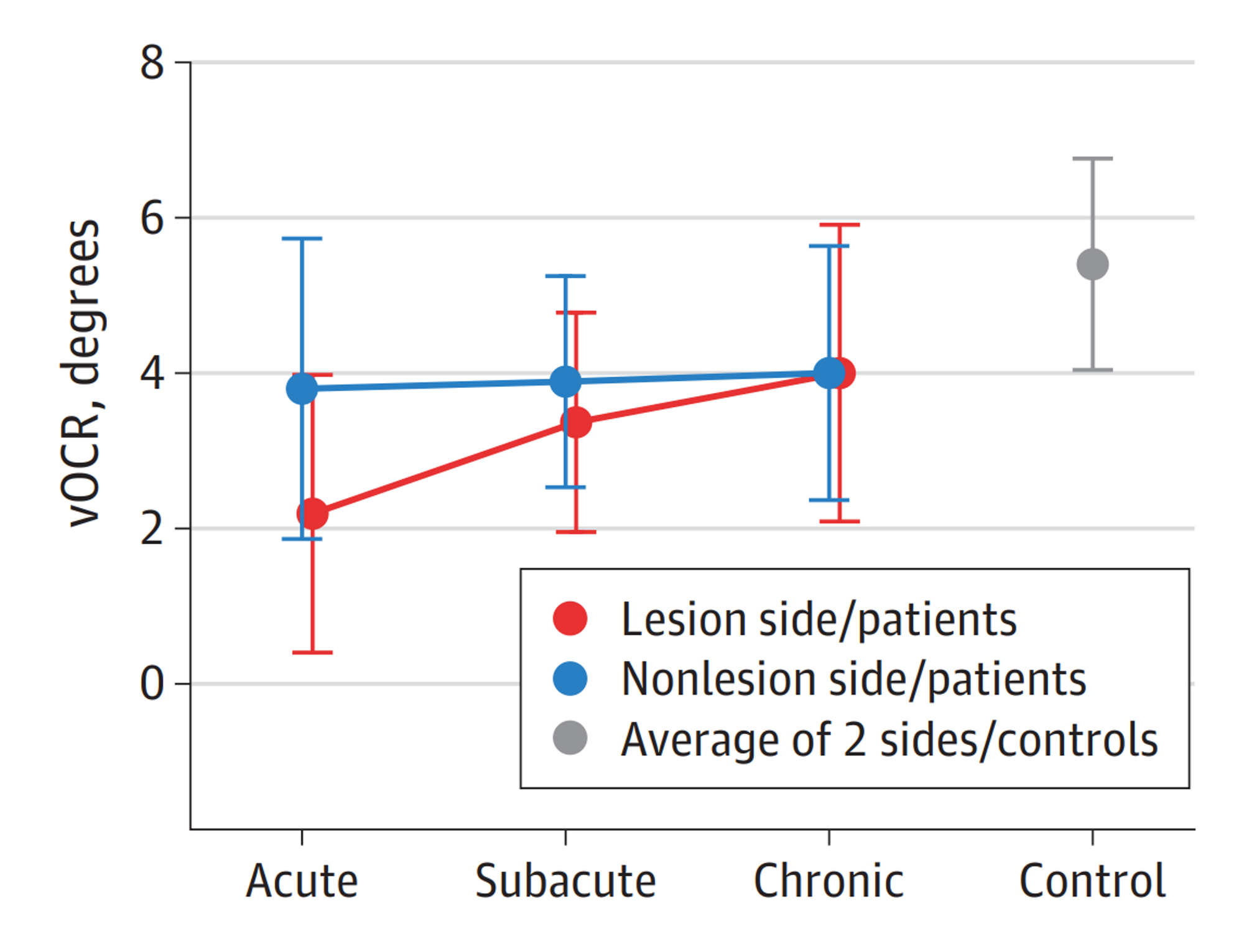
Results Of the 56 participants, 28 (50.0%) were men; mean (SD) age was 53.5 (11.4) years. The mean (SD) time of acute unilateral vestibular loss was 9 (7) days (range, 2-17 days) in the acute group, 61 (39) days (range, 28-172 days) in the subacute group, and 985 (1066) days (range 185-4200 days) in the chronic group. The vOCR test showed reduction on the side of vestibular loss, and the deficit was greater in patients with acute and subacute vestibular loss than in patients with chronic loss and healthy controls (acute vs chronic: −1.81°; 95% CI, −3.45° to −0.17°; acute vs control: −3.18°; 95% CI, −4.83° to −1.54°; subacute vs chronic: −0.63°; 95% CI, −2.28° to 1.01°; subacute vs control: −2.01°; 95% CI, −3.65° to −0.36°; acute vs subacute: −1.17°; 95% CI, −2.88° to 0.52°; and chronic vs control: −1.37°; 95% CI, −2.96° to 0.21°). The asymmetry in vOCR between the side of vestibular loss and healthy side was significantly higher in patients with acute vs chronic loss (0.28; 95% CI, 0.06-0.51). Overall, the performance of the vOCR test in discriminating between patients with vestibular loss and healthy controls was 0.83 (area under the receiver operating characteristic curve). The best vOCR threshold to detect vestibular loss at the 30° tilt was 4.5°, with a sensitivity of 80% (95% CI, 0.62%-0.88%) and specificity of 82% (95% CI, 0.57%-1.00%).
Conclusions and Relevance The findings of this case-control study suggest that the vOCR test can be performed with a simple bedside maneuver and may be used to detect or track loss of otolith function.
Citation
JAMA Otolaryngol Head Neck Surg. Published online March 25, 2021
Broad Topic
Diagnosis
Ocular motor control